Home Care: Safer and Faster
Recovery
Home care is planned health care and support given at home by family
caregivers, with professional help as required. The aim is to keep the patient
safe, comfortable, and as independent as possible while minimising hospital
visits and admissions.
When is Home Care suitable?
Home care is not for emergencies but for clinically stable patients who can be
safely managed at home with proper planning and support. Doctors should
always advise and reconfirm whether home care is clinically safe.
Common situations:
- Post‑hospitalisation: After surgeries, strokes, fractures, cardiac events,
or prolonged ICU stays, when the patient is stable but needs continued
nursing, wound care, physiotherapy, or rehabilitation.
- Senior citizens / geriatric care: Elders with limited mobility, multiple
chronic diseases (diabetes, hypertension, heart failure, COPD), or early
dementia who need regular monitoring and help with daily tasks.
- Long‑term conditions: People needing long-term tube feeding, catheter
care, tracheostomy care, or pressure sore prevention can often be
managed at home with trained support.
- Palliative and end‑of‑life care: Patients with terminal cancer or end-
stage organ failure who prefer comfort-focused care and symptom relief
at home.
Situations where home care will NOT be appropriate:
Unstable patients needing ICU care, ventilator support without reliable backup,
or continuous complex interventions, and homes where basic safety (electricity,
water, space, hygiene) cannot be ensured, and risks cannot be mitigated.
Advantages of Home Care
Home care has several practical benefits for patients and families when done
safely and correctly.
- Being at home reduces stress and anxiety, which often supports better
healing and well‑being.
- Avoiding long hospital stays reduces exposure to resistant germs and
hospital infections.
- Home care can be significantly cheaper than staying in a hospital for
weeks, especially for long‑term nursing care.
- Family members can stay close, learn caregiving skills, and participate in
decisions, which can improve outcomes and satisfaction.
- Minimises repeated trips to hospital OPDs, which is especially helpful for
bed‑bound patients or those living far from hospitals.
- Care can be customised to the patient’s routine, culture, and food
preferences.
Preparing the Home Environment and Infrastructure
Good preparation is essential to keep the patient safe at home and prevent harm.
Families should plan before bringing the patient home.
- Choosing the Right Room and Layout: Select a well-ventilated, well-
lit, and accessible room, with space around the bed for the caregiver and
equipment like a wheelchair, commode, etc. Keep essential items (a call
bell or mobile phone, medications, and emergency numbers) within reach
- Safe Bed: Use a firm, comfortable bed. In cases of high-risk patients, a
hospital-type bed with adjustable height and side rails may be needed.
Avoid cluttered furniture and sharp edges.
- Fall Prevention and Mobility Safety: Keep floors dry, avoid loose rugs.
Ensure good lighting in the toilet and passages. Install grab bars in toilets.
Consider a raised toilet seat or bedside commode for patients with poor
mobility.
- Hygiene and Infection Prevention: Ensure regular cleaning of the room
and bed rails with simple household disinfectants. Learn correct
techniques for wound care, catheter care, and tube feeding from a nurse
or doctor, and use sterile supplies as advised
- Safe Medication Management: Maintain a written medication chart
with drug name, dose, timing, and purpose; update it after every doctor
visit. Use pill organisers or alarms for patients with multiple medicines.
- Emergency Preparedness: Keep a list of emergency phone numbers
(ambulance, nearby hospital, treating doctor, key family members)
clearly displayed in the patient's room. Prepare a small emergency folder
with recent prescriptions, discharge summary, investigation reports, and
ID documents for quick hospital transfer if required. Know the early
warning signs that need urgent medical attention.
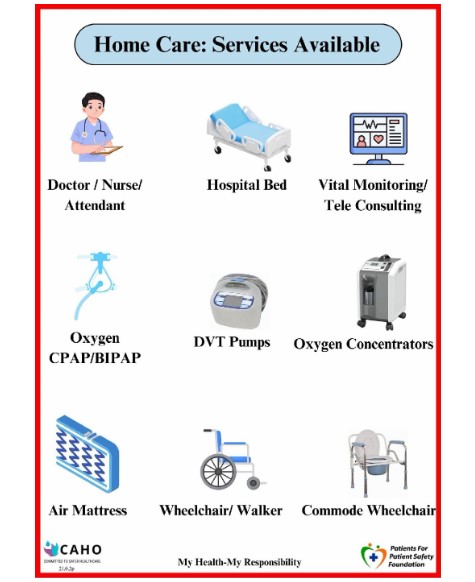
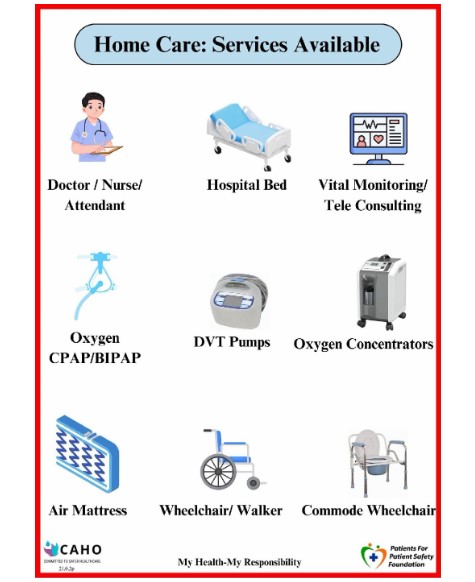
Services that can Support Home Care
Many larger hospitals and private home care agencies now offer structured
home care or hospital-at-home services.
- Periodic doctor home visits or video consultations for follow‑up.
- Trained nurses for wound dressing, injections, IV fluids, catheter care,
tracheostomy care, and monitoring vital signs.
- Physiotherapy at home for stroke, fractures, joint replacements, and
chronic pain.
- Palliative care teams for pain management, symptom control,
counselling, and end‑of‑life care planning.
- 24‑hour or 12‑hour home nurses/caretakers (for personal care, feeding,
turning, basic monitoring).
- Rental of equipment: hospital beds, wheelchairs, walkers, oxygen
concentrators, suction machines, BiPAP/CPAP devices, commodes, air
mattresses, and monitors.
Home care could speed up recovery and reduce the risk of infections and
other harm.