
Breast Cancer - Symptoms, Detection and Treatment
Introduction to Breast Cancer
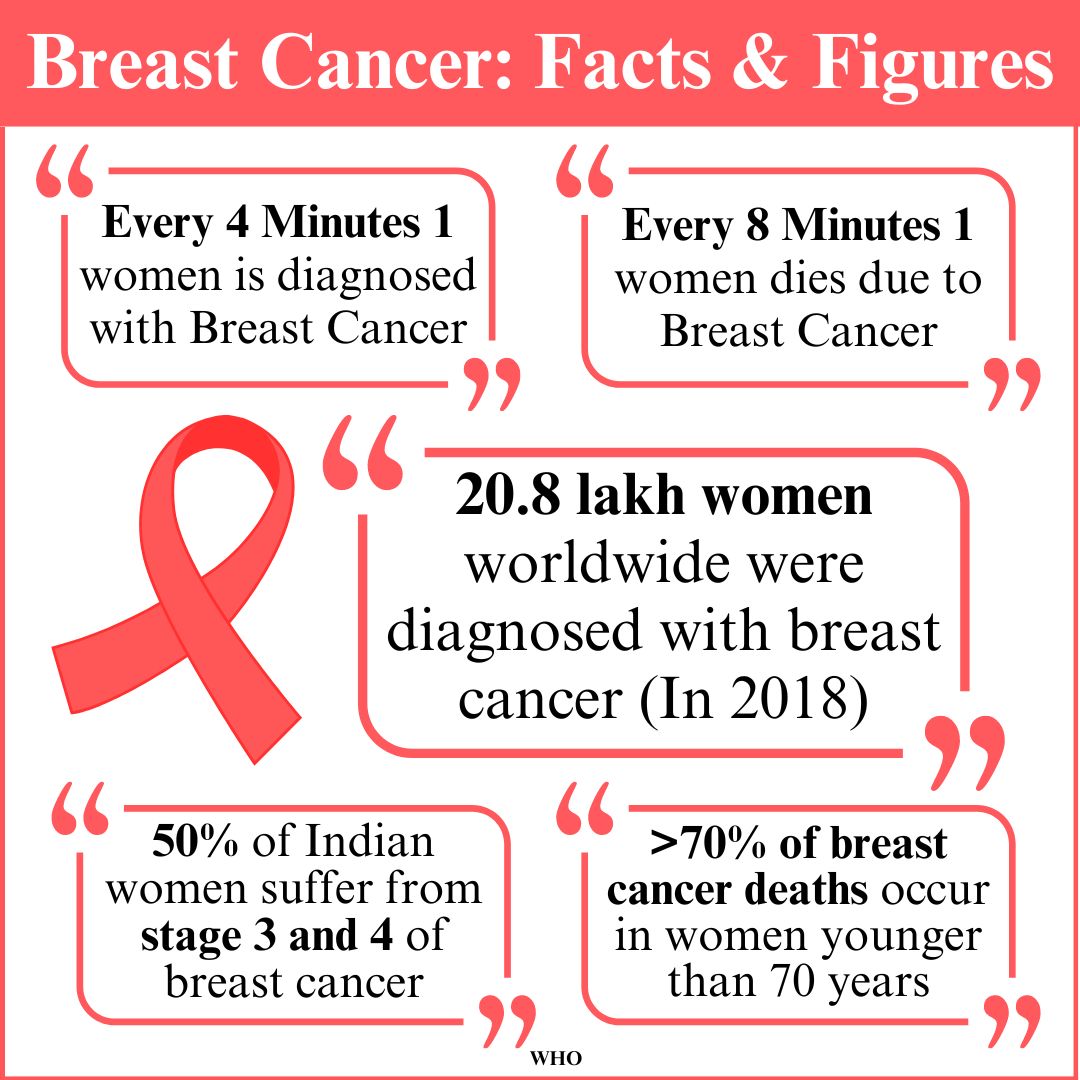
Breast cancer is the world’s most commonly diagnosed cancer among women, where abnormal breast cells grow out of control and form tumours. Most breast cancers begin in the milk ducts or lobules and they may spread outside the breast through blood vessels and lymph vessels. This is called metastasis. If left untreated, the tumours can spread throughout the body leading to complex treatments that can be fatal. Early detection and intervention can ensure high recovery and survival rates. There are significant research and advancement in medical science leading to effective treatment and outcomes.
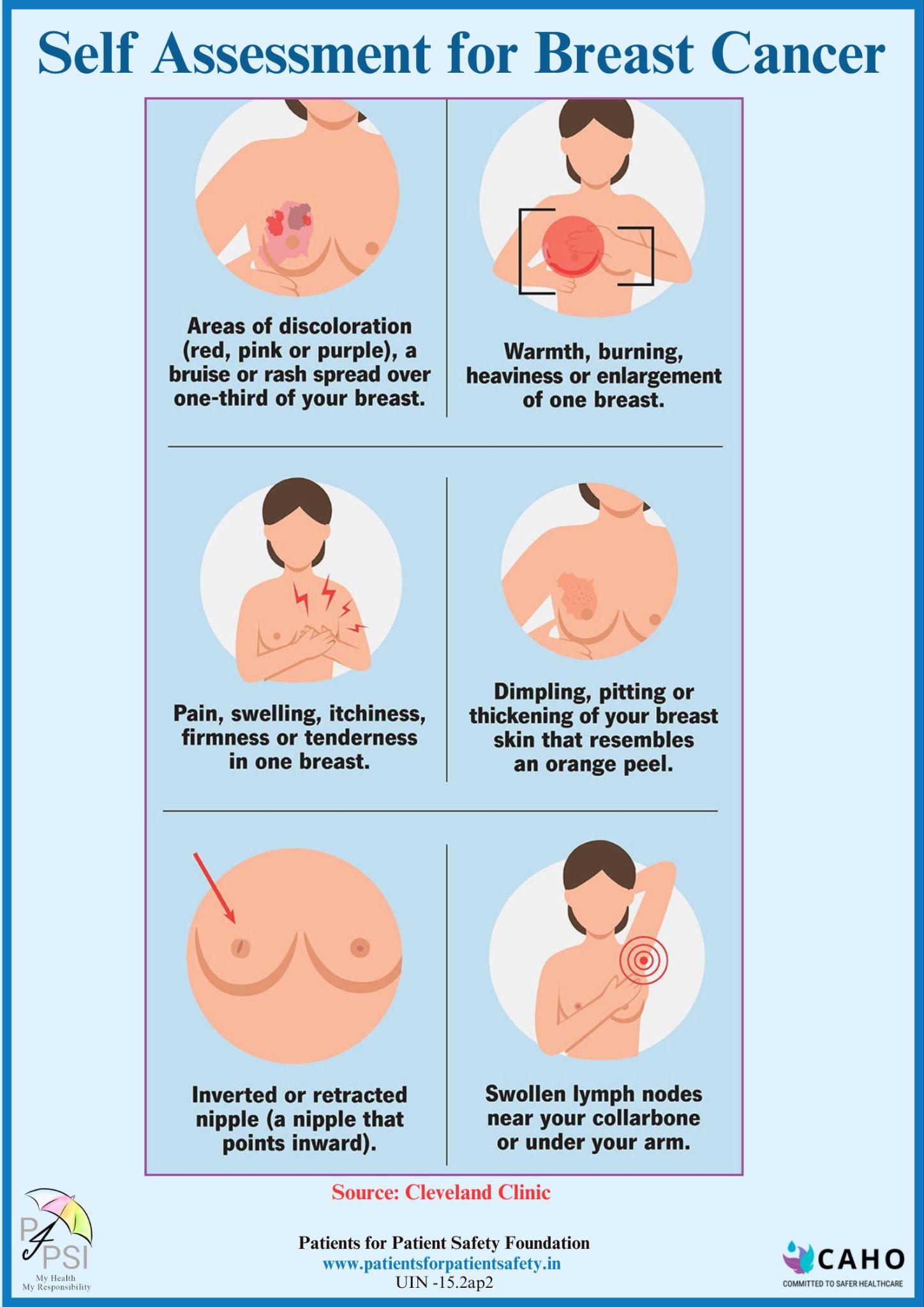
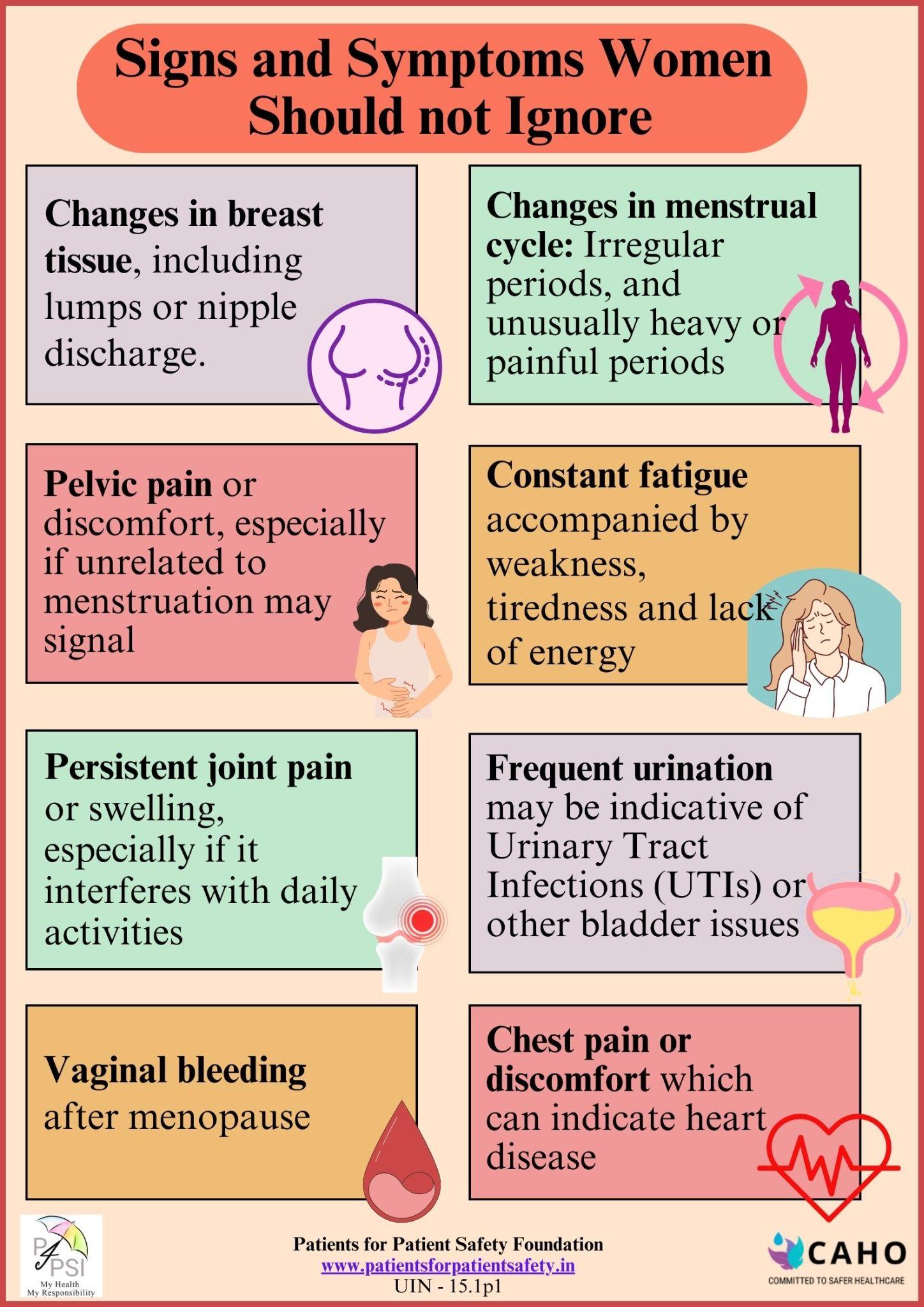
Signs and symptoms of Breast Cancer include:
- Lump thickening or swelling in the breast or underarm
- Unexplained changes in the size or shape of the breast
- Changes in skin texture such as redness, dimpling or puckering
- Nipple changes such as inversion, scaling, or discharge (other than breast milk)
- Pain in the breast or nipple

Consequences:
The most significant complication is metastatic when it spreads to other areas of the body, including the brain, bones, liver and lungs.
Causes and who is at risk:
Any woman can have a higher risk of breast cancer due to certain factors such as:
- Reproductive history:Starting menstrual periods before age 12 and starting menopause after age 55 expose women to hormones longer, raising their risk of getting breast cancer.
- Family history of breast:or ovarian cancer. A woman’s risk for breast cancer is higher if she has a mother, sister (first-degree relative) or multiple families who have had breast or ovarian cancer.
- Age:The risk for breast cancer increases with age. Most breast cancers are diagnosed after age 50. But happened earlier too.
- Radiation exposure: Having received excessive radiation treatments as a child or young adult.
How to detect:
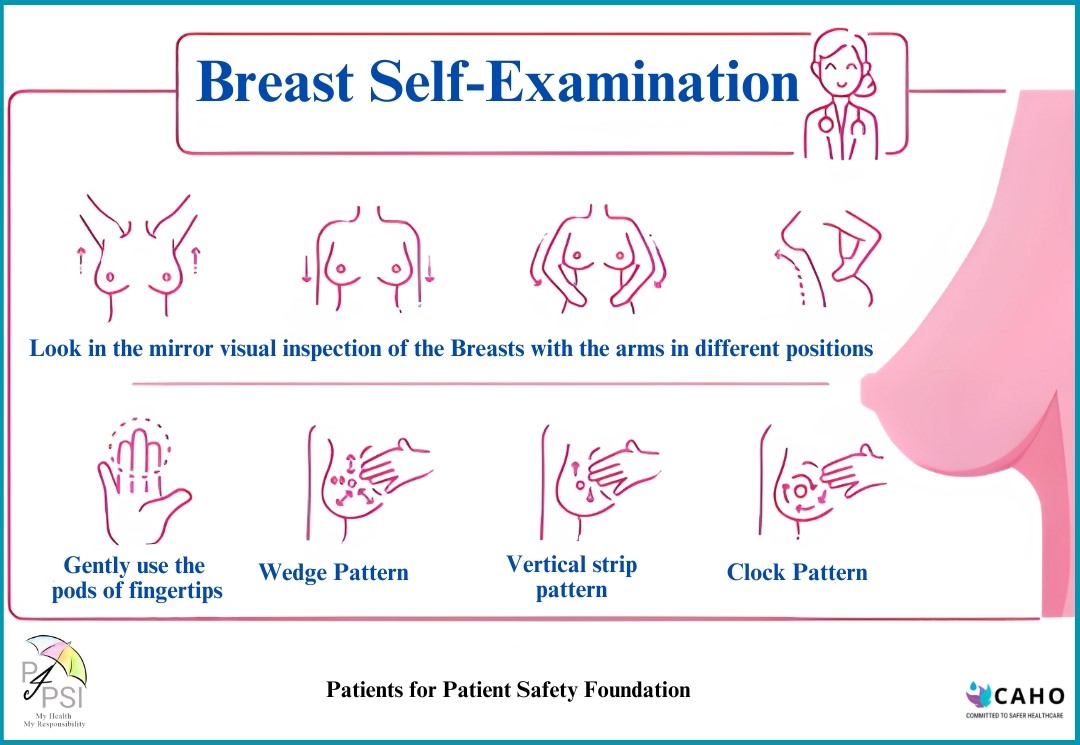
- Self-examination: Note any changes, lumps, or abnormalities during self-exams and report them to a healthcare professional.
- Breast ultrasound may give your healthcare team more information about a breast lump. For example, an ultrasound might show whether the lump is a solid mass or a fluid-filled cyst. The healthcare team uses this information to decide what tests you might need next
- Breast MRI can make more detailed pictures of the breast. Sometimes this method is used to look closely for any other areas of cancer in the affected breast. It also might be used to look for cancer in the other breast. Before a breast MRI, you usually receive an injection of dye. The dye helps the tissue show up better in the images.
- A mammogram is an X-ray of the breast tissue. Mammograms are commonly used to screen for breast cancer. If a screening mammogram finds something concerning, you might have another mammogram to look at the area more closely. This more detailed mammogram is called a diagnostic mammogram. It's often used to look closely at both breasts.
- Removing a sample of breast cells for testing to confirm whether there is cancer or not, a sample of tissue is removed from the breast.
Treatment options:
The Oncologist will decide the treatment protocol based on the stage, history, and overall health condition:
- Surgery to remove the tumour or full mammary glands. Remember prosthetic breasts can be used safely in case of full surgery.
- Radiation therapy to reduce recurrence risk in the breast and surrounding tissues
- Chemotherapy (chemo) uses drugs that are injected through veins or taken by mouth to kill cancer cells. There are several drugs used for chemo individually or in combination.
- Medications to kill cancer cells and prevent spread, including hormonal therapies or targeted biological therapies.
- Long-term medicines are now available for preventing recurrence. A healthy diet, regular exercise, and being stress-free enhance the chances of reducing recurrence.
How to reduce the risk of breast cancer and detect it early
- Breastfeed children if possible. Breastfeeding may have a protective effect against breast cancer.
- Self-examination: Note any changes, lumps, or abnormalities during self-exams and report them to a healthcare professional.
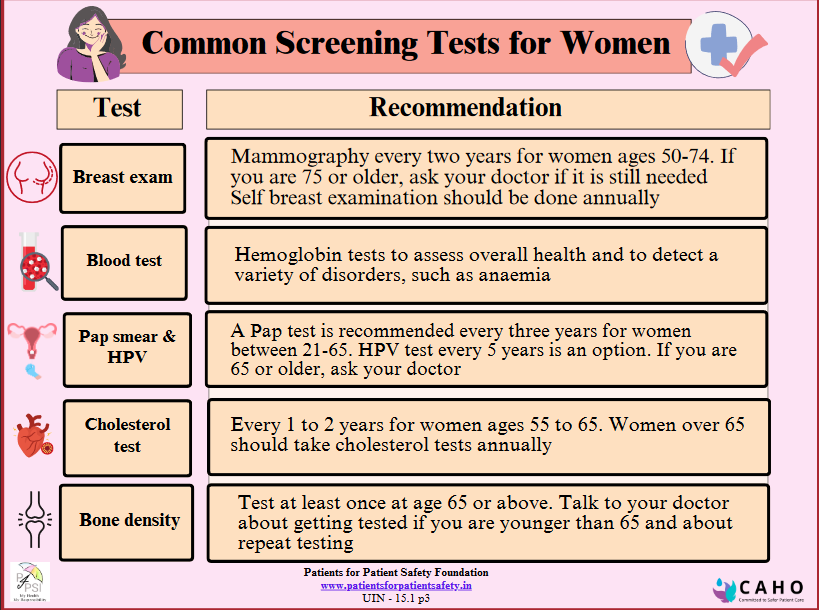
- Regular breast health checks: Be aware of changes in breasts and conduct clinical screening and mammograms, for early detection. Mammography regularly after 40 years.
- Advance screening, breast ultrasounds, and breast MRI as recommended by your physician, for early detection.
- With a family history of breast cancer discuss with your healthcare provider to determine if additional screening or preventive measures are necessary.
Cancer is treatable. You can lead a healthy long life. After you have been diagnosed. If treatment for it. The key is alert detection. Consult with your healthcare provider for personalised advice based on individual health history and risk factors.
 Back
Back